The benefits of patient centered care cannot be overestimated. But engaging and recognizing the stigma and embarrassment associated with bladder and bowel issues is essential – how can healthcare professionals best serve their patients?
It’s becoming more widely recognized that a holistic approach to bladder and bowel issues improve the symptoms and functioning in both areas. So what does that practically mean for the specialists involved in an individual’s care?
Many patients are never asked
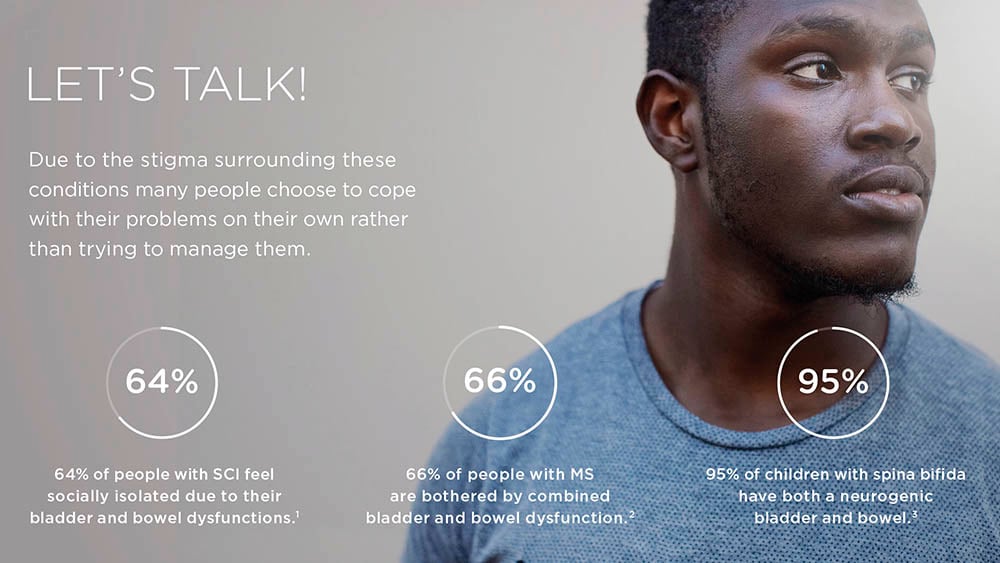
The stigma that surrounds symptoms of neurogenic bowel and bladder needs to be recognized as a factor in obstructing the best care. Patients often endure their symptoms as they may find it embarrassing to discuss. Their healthcare professional may not be making the connection between their bladder and bowel symptoms – incontinence, retention, constipation, urinary tract infections etc. The negative impact upon quality of life can lead to anxiety and depression.
Consider these two statements:
It was such a relief when I found my bladder and bowel therapies. Now I can leave the house, and start living my life again.
– Lee, 30, who has Multiple Sclerosis (MS)
It is so obvious to me that my bladder and bowel interact, affecting my health and well-being.
– Michael, 35, who has a Spinal Cord Injury (SCI)
Both Lee and Michael attribute a recovered sense of confidence and well-being to having had a holistic approach to their respective conditions.
How can healthcare providers improve their services?
We spoke to two specialists who have recognized that healthcare providers need to be doing more to further enhance the well-being of their patients.
– In a study with patients suffering from neurological damages we saw that those with a high Spinal Cord Injury or Spina Bifida had the worst bladder and bowel function. It’s rare to find someone with an awful bladder function whose bowel works optimal. Most times both are mild to severely affected, says Anne Cameron, Associate Professor of Urology at University of Michigan.
If the bladder and bowel are working, it makes you confident in leaving the house, going to your place of work, and having intimate relationships.
As a doctor you can assess patients with more dignity.
Since there is a lot of embarrassment involved, these patients need to have someone who understands their whole situation. Knowledge in both leads to better assessments and services.
– Anton Emmanuel
Anton Emmanuel is Senior Lecturer in Neuro-Gastroenterology at University College London and both of these experts are convinced that there are synergies well worth considering in the treatment of patients with neurogenic bladder and bowel.
– Teams separately involved in bladder treatment and bowel treatment need to understand their counterpart's management planning. You don’t need to be an expert, but you need to at least understand the basic principles, says Anne Cameron.
Anton Emmanuel agrees and develops:
– Staff are trained and specialized in areas of anatomy, rather than around diagnosis. To specialize in both disciplines is rare.
They share the concern that these specialties rarely meet in practice – other than in specialist centers for people with Spinal Cord Injury or other neurological diagnoses, and both are wholly convinced that collaboration must be an aspiration for all units involved in a patient’s care.
Examples of a combined approach to bladder and bowel
Therapies that relieve one condition often ease the other at the same time.4, 5, 6 For example, the number of urinary tract infections (UTIs) and urinary incontinence episodes may decrease significantly with the addition of a bowel management program for people with bladder dysfunction.4, 7
Some therapies can be effective for combined bladder and bowel dysfunction; sacral neuromodulation is one example.5
– I practice sacral neuromodulation therapy. It’s an identical procedure, performed the same way for fecal incontinence as for urinary incontinence. And it fixes both. It was designed for bladder care, but a side effect is that it took away the fecal incontinence. Now it's an approved therapy for both, says Anne Cameron.
Treating someone’s bladder doesn’t make their bowel better, and treating their bowel doesn’t make their bladder better, but treating them both as a whole does treat the person
– Anne Cameron
Watch Anne and Anton discuss how they discovered the benefits of a combined bladder and bowel strategy.
- Van der Meer et al., Spinal Cord. 2017;55:98-104.
- Wang et al., Mult Scler Relat Disord. 2018;20:16-21.
- Zickler & Richardsson, J Ped Health Care. 2004;18:276-283.
- Radojicic et al. BJU Int. 2018. doi:10.1111/bju.14414
- Chen and Liao. Spinal Cord. 2015;53:204-208.
- Rasmussen et al. Ugeskr. Laeger. 2011;173(39):2412-2415.
- Radojicic et al. J. Pediatr. Urol. 2018. doi: 10.1016/j.jpurol.2018.05.025




